In a refreshingly candid conversation with Oprah Daily Insiders, Oprah, Maria Shriver, Drew Barrymore, and doctors Sharon Malone, Heather Hirsch, and Judith Joseph, we set the record straight on all things menopause. Become an Oprah Daily Insider now to get access to this conversation and the full "The Life You Want” Class library.
If you’re in your mid-30s, menopause is probably the last thing on your mind—just a distant, “I’m in my 40s” kind of thing, like shopping for reading glasses or watching HGTV. But if you notice that your periods are starting to veer off schedule, or you’re struggling to sleep, breaking out like a teenager, or feeling moody, you may be entering “perimenopause,” i.e. the prelude to the big M.
More From Oprah Daily

Also known as the “menopause transition,” perimenopause encompasses the years of hormonal fluctuations leading up to the day you’ve gone 12 months without your period. (Incidentally, that single day is what’s known as menopause—yes, just that one day.) It typically begins for women ages 40 to 44, but it can start in your 30s, and lasts an average of four to eight years.
In most cases, starting the transition in your mid-30s is nothing to freak out about, says Suzanne Gilberg-Lenz, MD, the author of Menopause Bootcamp. “Just be aware that another developmental phase is coming, and it’s a natural process. Having said that, [symptoms] that are very disruptive or uncomfortable deserve to be addressed.” Your main MD or ob-gyn might be able to alleviate these growing pains, and you also want to rule out any unrelated medical condition that could be causing problems, she explains. But first, the facts:
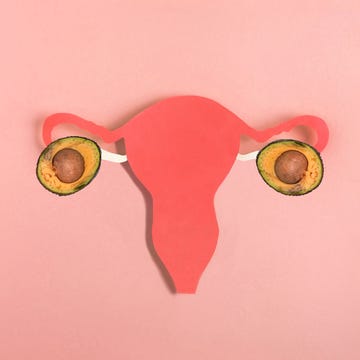
1. Perimenopause is basically adult puberty
During the menopause transition, your hormones, specifically ovary-produced estrogen and progesterone, fluctuate rather unpredictably, eventually dwindling and vanishing altogether. Think of it like the hormonal chaos that happened in high school, but instead of prepping you for your reproductive years, your body is phasing out of them, says Jen Gunter, MD, the author of The Menopause Manifesto. This “midlife puberty,” as Gilberg-Lenz likes to call it, can manifest in a whole bunch of annoying, unpleasant symptoms that vary widely from person to person.
Here are a few you may experience:
- Irregular menstrual periods
- Heavier or lighter periods
- Hot flashes or just feeling hotter in general
- Insomnia
- Brain fog
- Dry and/or pimply skin
- Anxiety and/or depression
- Vaginal dryness
- Worsening PMS symptoms (bloating, breast tenderness, cravings, mood swings, etc.)
Many of these symptoms are par for the course in your 40s. But if you’re younger, your MD will probably screen to make sure something else isn’t going on. For instance, irregular periods and dry skin could be a sign of a thyroid disorder, says Gunter, and heavier bleeding might indicate that you have a fibroid, says Gilberg-Lenz, adding that “it’s important to partner with a knowledgeable physician to help you unwind all of this.”
2. You can’t really test for it
There are several at-home blood tests sold online claiming to analyze your hormone balance and tell you how close to menopause you are. They typically monitor levels of estrogen, luteinizing hormone, and follicle-stimulating hormone, all important for ovulation. But just like you didn’t need a lab to know that you were in puberty, you don’t need one to tell you you’re in perimenopause, says Gunter. Perimenopause is generally diagnosed clinically, she adds, meaning that your doctor will factor in your age, medical history, family history, and symptoms.
Plus, one blood test won’t account for the unpredictable rise and fall of hormones during your transition. “So when you’re doing it, you never know where you’re catching somebody,” says Gunter. “You could literally catch somebody in their very last menstrual cycle and they could have totally ‘normal’ hormone levels, or catch someone who ‘looks’ like they are in menopause, and then three months later, they ovulate.”
3. Genes and race can impact the timing, duration, and severity of symptoms
Recent studies have shown that genetics and family history play a major role in determining the age you reach menopause. “If everybody in your family went through it early, chances are you might as well,” says Gilberg-Lenz. Women of color also tend to start perimenopause earlier and have more severe hot flashes than white women, according to the SWAN study, which followed a racially, ethnically, and geographically diverse group of 3,302 premenopausal women. On top of that, Black and Latina women experience perimenopause symptoms about two to four years longer than white women.
The reasons for these variations are complex, since factors like socioeconomic status, quality of life, access to education, and immigration status all play a role. And in general, stress and anxiety have been known to worsen hot flashes. Fortunately, there are expanding networks of POC physicians dedicated to serving their communities.
4. Perimenopause messes with your sex drive
So you haven’t been feeling it with your partner lately. Part of the reason may be that testosterone declines during the menopause transition, but to “boil sex drive down to testosterone is ridiculous,” says Gilberg-Lenz, who stresses that libido is multifaceted: It’s affected by your energy and stress levels and the sense of connection (or lack of connection) you have with your partner.
Perimenopause can also make sex less pleasurable or even uncomfortable. Estrogen helps to keep the vagina lubricated, so when it’s diminishing, intercourse can be painful, according to the American College of Obstetricians and Gynecologists. As if that weren’t enough of a downer, changes in blood flow and the nerves in the vagina can hamper its response time to pleasure, says Gilberg-Lenz. Thankfully, there are easy fixes. Lube can help to add moisture, and vibrators have been proven effective in improving blood flow to the vagina. For extreme dryness, you can ask your doctor about vaginal estrogen in the form of a suppository or cream.
Talking to a shrink can do wonders, too, says Gunter. Cognitive behavioral therapy and mindfulness-based therapy can help you stay present during sex and manage any triggering thoughts or emotions that come up and kill the mood. Research shows that both methods are “better than any libido-specific medication,” she says.
5. It goes hand in hand with declining fertility
We know by now that women can conceive in their late 40s, and sometimes beyond. “I have had patients come in at 46, 47 and have totally healthy pregnancies,” says Gilberg-Lenz. This is why, if you’re not trying to have children, you continue to use birth control until your periods have stopped.
But we also know a parallel truth: that your chances of carrying a baby to term gradually decrease after the age of 35. This is because not only do the number of eggs you have available decrease, but your ovaries become less responsive to the hormones that make you ovulate, according to the Women’s Health Research Institute. The bottom line: “If you're 35, don’t wait till you’re 43 to have a conversation with a fertility specialist,” says Gunter. “It’s good to be armed with information.”
6. Regular exercise helps offset the health risks
Those risks include bone disease, heart disease, and dementia. Yikes.
If there’s one piece of advice Gunter could give to anyone in their 30s, it’s to start strength training now, when you’re still producing estrogen, a hormone that is essential to maintaining healthy bones. When levels drop, your risk of developing osteoporosis—a condition in which the bones become brittle—increases, according to experts at the Endocrine Society. Your risk of conditions like dementia and heart disease increases during perimenopause because of various changes that happen in your circulation and brain.
The good news: “If you look at all the conditions that increase with menopause, almost every single one of them improves with exercise,” says Gunter. Weightlifting or weight-bearing exercise (like walking or doing push-ups) can strengthen your bones well into old age, so aim to strength-train at least twice a week. Additionally, the Department of Health and Human Services suggests moderate cardio (like walking) at least 150 minutes a week or vigorous cardio (i.e. a kickboxing class) for at least 75 minutes a week.
7. You don’t have to suffer in silence
While perimenopause is not a disease to be treated, there are plenty of things your doctor can suggest to make the ride a little smoother. For example, studies have shown that birth control and antidepressants can help reduce heavy bleeding and hot flashes. Stress reduction (via yoga, meditation, or working with a therapist) can also ease symptoms, according to experts at the Mayo Clinic.
Whatever your symptoms, keep your doctor in the loop, and don’t downplay them. The more aware you both are about the changes happening in your body—from the mildly annoying to the most debilitating—the better equipped you’ll be to sail through this hormonal storm to calmer (we promise!) shores.
Any content published by Oprah Daily is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. It should not be regarded as a substitute for professional guidance from your healthcare provider.
In a refreshingly candid conversation with Oprah Daily Insiders, Oprah, Maria Shriver, Drew Barrymore, and doctors Sharon Malone, Heather Hirsch, and Judith Joseph, we set the record straight on all things menopause. Become an Oprah Daily Insider now to get access to this conversation and the full"The Life You Want” Class library.